Entendiendo la importancia del tiempo adecuado entre cada sesión de radioterapia (descansos y exposición al haz de radiación)

Por: Dr Rolando Loría

La Radioterapia es un tratamiento comúnmente utilizado en el manejo de varios tipos de cáncer. La radiación se administra en fracciones (sesiones) para maximizar el daño a las células cancerosas mientras se minimiza el impacto en los tejidos normales circundantes. La tasa de muerte celular es un aspecto crucial en la eficacia del tratamiento de radioterapia.
Cuando hablamos del término médico «intervalos elongados intra fracción», nos referimos a la separación de tiempo entre las dosis de radiación dentro de un tratamiento. La administración de dosis fraccionadas permite que las células normales tengan tiempo para reparar el daño causado por la radiación, mientras que las células cancerosas, que a menudo tienen una capacidad de reparación más limitada, pueden acumular daño y eventualmente morir (Shibamoto, Miyakawa, Otsuka, & Iwata, 2016).
Si los tiempos entre las dosis son muy cortos, las células normales pueden no tener suficiente tiempo para recuperarse, lo que puede aumentar el riesgo de efectos secundarios. Por otro lado, si los intervalos son demasiado largos, las células cancerosas pueden tener tiempo para reparar parte del daño, reduciendo la eficacia del tratamiento.
Los tiempos promedio entre cada sesión de radioterapia dependerán de la dosis y el esquema de tratamiento sin embargo el tiempo mínimo de “descanso” entre una sesión y otra es aproximadamente de 6 horas en lesiones de Cerebro y 8 horas en lesiones de cuerpo.
Los tiempos máximos de “descanso” variarán entre las 24 o 48 horas entre cada sesión según el esquema de tratamiento indicado.
TIEMPO DE EXPOSICIÓN
Sumado a esto, existe otra variable importante a considerar: los tiempos de exposición a la radiación durante los tratamientos.
El experto Khorramizadeh y colaboradores demostraron que cuando el tiempo de exposición al haz de radiación por sesión aumenta de 15 minutos a 45 minutos en cada fracción (sesión de tratamiento), la muerte de las células tumorales se reduce. Parece que el fenómeno principal que afecta la respuesta celular es la reparación al daño subletal. El efecto de la dosis administrada durante 15 minutos puede ser mayor que el de 30 y 45 min (Khorramizadeh, Saberi, & Tahmasebi-Bi, 2017).
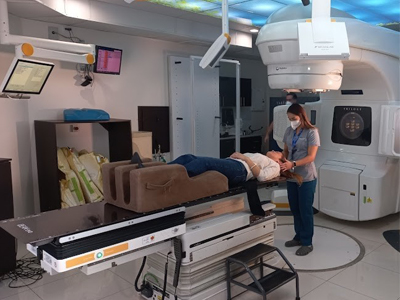
Equipos de altas dosis como el Acelerador Lineal con el que cuenta el Centro Médico de Radioterapia Siglo XXI, permiten entregar dosis de radiocirugía de forma sumamente exacta en los periodos máximos indicados en estos estudios, logrando no solamente el daño celular esperado sino contribuyendo con la comodidad del paciente a no ser expuesto a largos periodos de tratamiento como sucede en otros equipos de radiocirugía.
La tasa de muerte celular en radioterapia depende de varios factores, incluyendo la sensibilidad de las células al daño por radiación, el tipo de radiación utilizada, la dosis total administrada y la fracción de dosis. La relación entre la tasa de muerte celular y los intervalos intra fracción específicos puede variar según el tipo de cáncer y el tratamiento (Benedict, Lin, Zwicker, Huang, & Schmidt-Ullrich, 1997).
Es importante señalar que la planificación de tratamientos de radioterapia se realiza de manera personalizada para cada paciente, teniendo en cuenta diversos factores clínicos y radiobiológicos. Los oncólogos radioterapeutas trabajan para optimizar la administración de la radiación para lograr la máxima eficacia contra el cáncer mientras minimizan los efectos secundarios en los tejidos normales.
Bibliografía
Khorramizadeh, M., Saberi, A., & Tahmasebi-Bi, M. (1 de sep de 2017). Impact of Prolonged Fraction Delivery Time Modelling Stereotactic Body Radiation Therapy with High Dose Hypofractionation on the Killing of Cultured ACHN Renal Cell Carcinoma Cell Line. J Biomed Phys Eng(3), 205-216.
Shibamoto,, Y., Miyakawa, A., Otsuka, S., & Iwata, H. (2016). Radiobiology of hypofractionated stereotactic radiotherapy: what are the optimal fractiona- tion schedules? J Radiat Res .(57 Suppl 1), 76-i82.
Benedict, S., Lin, P., Zwicker, R., Huang, D., & Schmidt-Ullrich, R. (1 de Mar de 1997). The biological effectiveness of intermittent irradiation as a function of overall treatment time: development of correction factors for linac-based stereotactic radiotherapy. Int J Radiat Oncol Biol Phys ., 37(4), 765-9.