Cáncer de Próstata

¿Qué es el cáncer de próstata?
El cáncer de próstata es el segundo tipo de cáncer más común entre los hombres en los Estados Unidos, y de acuerdo a la incidencia en Costa Rica entre el periodo comprendido desde el año 2000 a 2015, también fue el cáncer de próstata el más frecuente en varones, seguido por el de piel, estomago, colon y pulmón.
La próstata es una glándula que sólo tienen los hombres por lo tanto pertenece al sistema reproductor masculino, está localizada justo debajo de la vejiga y delante del recto. El cáncer de próstata se origina cuando las células de la próstata comienzan a crecer fuera de control.
¿CÓMO SE PUEDE DIAGNOSTICAR EL CÁNCER DE PRÓSTATA?
Los exámenes más comunes para el cáncer de próstata son:

TACTO RECTAL: Consiste en un examen mediante el cual el médico se coloca un guante lubricado y por vía rectal palpa la próstata a través de la pared rectal en busca de nódulos o áreas anormales. La glándula prostática se encuentra inmediatamente delante del recto, y la mayoría de los cánceres comienzan en la parte posterior de la glándula, lo que se puede palpar durante un examen del recto. Este examen es incómodo, pero no es doloroso y lleva muy poco tiempo realizarlo.
PRUEBA DE ANTÍGENO PROSTÁTICO: Mide el nivel del antígeno prostático específico, una proteína que se encuentra en la sangre de un hombre, producida por la glándula prostática. La probabilidad de tener cáncer de próstata aumenta a medida que el nivel de PSA sube. La mayoría de los hombres sin cáncer de próstata tiene niveles de PSA menores a 4 ng/mL de sangre. Cuando se forma el cáncer de próstata, el nivel de PSA a menudo aumenta a más de 4. Sin embargo, un nivel por debajo de 4 ng/ml NO garantiza que un hombre no tenga cáncer. Alrededor del 15% de los hombres que tienen un PSA menor de 4 presentará cáncer de próstata si se hace una biopsia.
BIOPSIA DE LA PRÓSTATA: La cual el médico obtiene tejido de la glándula para determinar si hay células cancerosas presentes. Para algunos hombres, hacer una biopsia de próstata podría ser la mejor opción, especialmente si el nivel inicial de PSA es alto. Esta prueba es la única forma de saber con seguridad si un hombre tiene cáncer de próstata. Si se encuentra cáncer de próstata en una biopsia, este examen también puede ayudar a indicar cuán probable es que el cáncer crezca y se propague rápidamente.
Si se encuentra cáncer de próstata en la biopsia, se le asignará un grado. El grado del cáncer se basa en qué tan anormal se observa el cáncer al microscopio. Esta prueba permitirá confirmar el diagnóstico de cáncer y nos dará idea del volumen tumoral y el grado de agresividad puntuación Gleason la cual ha estado en uso durante muchos años, asigna grados al comparar el cáncer con el tejido prostático normal:

SÍNTOMAS:
Necesidad de orinar a menudo, especialmente de noche
Dificultad para comenzar o detener el chorro de orina
Una expulsión de orina débil o interrumpida
Dificultad para orinar
Gotear orina al reírse o al toser
Dolor o ardor al orinar
Sangre en la orina o en el semen
Un dolor sordo o rigidez en la espalda baja, las costillas o la parte superior de los muslos
Inflamación, debilidad o entumecimiento de las extremidades inferiores (areola) o la piel de la mama, Enrojecimiento o pequeños orificios en la piel que se encuentra sobre tu mama, como la piel de una naranja.
TRATAMIENTO

Dentro de las técnicas que se utilizan y brindamos en Radioterapia Siglo XXI se encuentran:
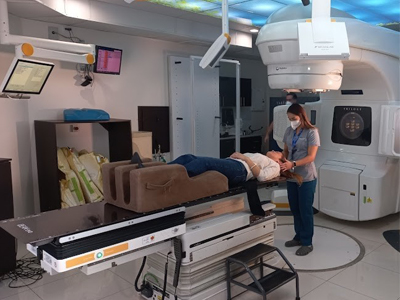
RADIOTERAPIA DE INTENSIDAD MODULADA (IMRT): Permite variar (escalar) la dosis de RT y la intensidad durante la terapia. Reduce los efectos secundarios y facilita el tratamiento cuando hay que incluir los ganglios linfáticos pélvicos en el campo. Permite administrar dosis muy elevadas (81 Gy) con poca toxicidad intestinal. Esta técnica emplea una máquina controlada por una computadora que se mueve alrededor del paciente a medida que emite la radiación. Además de configurar los rayos y dirigirlos a la próstata desde varios ángulos, la intensidad (fuerza) de los rayos puede ser ajustada para limitar las dosis de radiación que llegan a los tejidos normales adyacentes. Esto permite que los médicos suministren una dosis de radiación incluso más elevada al cáncer.
RADIOTERAPIA ESTEREOTÁXICA (SBRT): Consiste en administrar una dosis elevada de irradiación a nivel de la próstata mediante técnicas de radioterapia complejas y precisas. Actualmente los estadios tempranos pueden ser tratados con esta técnica de radioterapia en tan solo 5 días en nuestro centro con una mayor precisión sin aumentar los efectos secundarios del tratamiento.
RADIOTERAPIA GUIADA POR IMÁGENES (IGRT): Permite también la administración de dosis más altas de radioterapia externa (incluso llegar hasta 90Gy) mediante la utilización de técnicas de imagen avanzada como la resonancia magnética con espectroscopia o un escáner de imágenes integrado. Este adelanto le permite al médico tomar fotografías de la próstata justo antes de administrar la radiación para hacer ajustes menores en la dirección de los rayos. Esto parece ayudar a administrar la radiación incluso de forma más precisa, lo que conduce a menos efectos secundarios y es una técnica novedosa que se aplica en nuestro centro médico actualmente.
VIGILANCIA ACTIVA: Para estadios de muy bajo riesgo y bajo riesgo. Si usted y su médico están de acuerdo en que la vigilancia activa es una buena idea, su tratamiento incluirá visitas regulares al médico y pruebas de sangre para medir el antígeno prostático específico (PSA). Si el cáncer crece o si su condición cambia, su médico puede comenzar el tratamiento
Si el cáncer se ha extendido más allá de la próstata, los médicos usan tratamientos sistemáticos. Estos incluyen la terapia de hormonas, la quimioterapia y las vacunas para el cáncer de próstata.