Radioterapia Compensatoria de Movimiento 4D

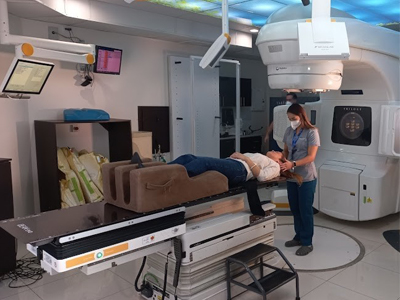
Radioterapia Compensatoria de Movimiento 4D, conocida también como “Radioterapia de Cuarta Dimensión”, tecnología que emplea el sistema RPM de Varian.
Esta modalidad permite monitorear, a la vez que se toman imágenes de tomografía computarizada en las diversas fases del ciclo respiratorio y de esta forma los médicos pueden elegir el momento más adecuado en este ciclo del paciente para activar el tratamiento.
El equipamiento nos permite optimizar el tiempo previo en la aplicación de los tratamientos que se hacen actualmente, ya que tiene la tecnología necesaria para proteger los órganos alrededor del área a irradiar, y además modular la intensidad a través del sistema integrado de colimador multihojas (MLC)
¿Quiénes participan en este procedimiento y quien maneja el equipo?
La mayoría de los centros médicos cuentan con un equipo de personal especialmente capacitado en la administración de IMRT. En este equipo participan el radioncólogo, el físico médico, el dosimetrista, los imagenólogos y el personal de enfermería de radioterapia.
El radioncólogo, un médico especialmente entrenado, primero consulta con el paciente para determinar si la radioterapia con IMRT es el tratamiento más adecuado. Luego de la obtención de consentimiento informado, se establece un curso de tratamiento individualizado. Un radiofísico, que tiene entrenamiento especializado en el campo de la física radioncológica, asegura que el acelerador lineal suministre la dosis precisa de radiación y que los cálculos computarizados de las dosis sean correctos. Un dosimetrista trabaja con el radiofísico médico para calcular las exposiciones a la IMRT y las configuraciones de haces necesarias para suministrar la dosis prescrita por el radioncólogo. El plan de tratamiento final es verificado por el físico médico, con mediciones en la máquina, antes de ser administrado al paciente. Un imagenólogo altamente especializado coloca al paciente en la mesa de tratamiento y maneja la máquina. La enfermera de radioncología evalúa al paciente sobre la mesa de tratamiento y le provee información adicional sobre el tratamiento y las posibles reacciones adversas. La enfermera de radioncología, en colaboración con el médico, también ayuda a controlar reacciones o efectos secundarios que pudieran presentarse.
- El imagenólogo maneja el equipo desde una zona cercana protegida de la radiación. El terapeuta puede comunicarse con el paciente durante todo el procedimiento, y puede observar al paciente a través de una ventana o por televisión de circuito cerrado.
- Un neurólogo o neuroncólogo puede participar con el oncólogo radioterapeuta y neurocirujano en el equipo multidisciplinario que considera varias opciones de tratamiento para casos individuales y ayuda a decidir quien puede beneficiarse de la radiocirugía para lesiones en el cerebro.
Preparaciones especiales necesarias para el procedimiento
Antes de la planificación de tratamiento, se hace un examen físico y se revisa la historia clínica. Luego, hay una sesión de simulación de tratamiento, en la que se hace una TC que le permite al radioncólogo especificar la forma tridimensional del tumor y de los tejidos normales. En la mayoría de los casos, puede ser necesaria una sesión de preparación de tratamiento para moldear un dispositivo especial que ayuda al paciente a mantener la posición de tratamiento exacta. Algunas veces, previamente a la simulación, se le indica al paciente que siga ciertos regimenes de preparación intestinales y de la vejiga. El dosimetrista y el médico usan la información de la TC para diseñar los haces de IMRT que, bajo especificaciones del oncólogo radioterapeuta, serán usados durante el tratamiento. A veces, durante la TAC se inyectan agentes de contraste intravenosos para ayudar a definir mejor el tumor. Ocasionalmente, otros procedimientos de diagnóstico, como la tomografía por emisión de positrones (PET) y la resonancia magnética nuclear (RMN), pueden ser necesarios para la planificación de la IMRT. Estas imágenes de diagnóstico pueden combinarse con la TC de planificación y ayudan al radioncólogo a determinar la ubicación exacta del tumor que se va a tratar. En algunos casos es necesario insertar marcadores de radio densos dentro del área objeto para posicionamiento más preciso. Por lo general, las sesiones de IMRT comienzan aproximadamente una semana después de la simulación. Antes del tratamiento, es posible que se marque o tatúe la piel del paciente con una tinta de color, lo que ayudará a alinear el equipo con la zona a tratar.
¿Qué se siente durante y después del procedimiento?
Al igual que con otros tratamientos de radioterapia con haces externos, no se espera que haya dolor durante el tratamiento en sí. Sin embargo, es posible parar la máquina si usted experimenta incomodidad debido a la posición de tratamiento o a los aparatos posicionadores. A medida que el tratamiento avanza, algunos pacientes pueden sufrir ciertos efectos secundarios relacionados con el tratamiento. La naturaleza de los efectos secundarios depende de cuáles estructuras de tejido normal se están irradiando. El radioncólogo y la enfermera hablarán con usted sobre esto y le ayudarán si tiene efectos secundarios.
Los efectos secundarios de la radioterapia incluyen problemas que ocurren como resultado del tratamiento mismo así como del daño hecho por el tratamiento a las células sanas en el área del tratamiento.
El número y la severidad de los efectos secundarios que usted experimenta dependen del tipo de radiación y la dosificación que recibe y la parte del cuerpo sometiéndose a tratamiento. Debe hablar con el medico y la enfermera acerca de cualesquiera efectos secundarios que experimenta para que puedan ayudarle a controlarlos.
La radioterapia puede causar efectos secundarios tempraneros y retardados. Los efectos secundarios tempraneros ocurren durante o inmediatamente después del tratamiento y normalmente desaparecen dentro de pocas semanas. Los efectos secundarios tempraneros comunes de la radioterapia incluyen cansancio o fatiga y problemas en la piel. La piel en el área de tratamiento puede ponerse más sensible, roja, irritada o hinchada. Otros cambios en la piel incluyen sequedad, picazón, exfoliación y formación de ampollas.
Según el área sometiéndose a tratamiento, otros efectos secundarios tempraneros pueden incluir:
- Pérdida de pelo en el área de tratamiento
- Problemas en la boca y dificultad en tragar
- Problemas en comer y en la digestión
- Diarrea
- Nausea y vómito
- Dolores de cabeza
- Sensibilidad e hinchazón en el área del tratamiento
- Cambios urinarios y en la vejiga
Los efectos secundarios retardados, que son raros, ocurren meses o años después del tratamiento y a menudo son permanentes. Incluyen:
- Cambios cerebrales
- Cambios en la columna vertebral
- Cambios pulmonares
- Cambios hepáticos
- Cambios en el colon y el recto
- Infertilidad
- Cambios en las coyunturas
- Linfedema
- Cambios en la boca
- Cáncer secundario
Existe un pequeño riesgo de desarrollar cáncer a causa de la radioterapia. Después de radioterapia para cáncer, usted debe someterse a un examen regular por su radioncólogo para detectar cánceres recurrentes y nuevos.
Usando técnicas tales como la IMRT, los oncólogos radioterapetas están maximizando las capacidades de la radioterapia para destruir el cáncer a la vez que se minimiza su efecto en los tejidos y órganos sanos y los efectos secundarios del tratamiento mismo.