Cáncer Cérvix

¿Qué es el cáncer Cérvix?
El cáncer de cérvix se inicia cuando las células sanas de su superficie comienzan a dividirse de manera descontrolada. Estos cambios condicionan anomalías, no necesariamente cancerosas. Estos son los primeros pasos que pueden dar lugar a la formación de un cáncer.
El cáncer de cuello uterino, o de cérvix, se ubica entre los más frecuentes en la población femenina a nivel mundial, y según estadísticas del World Cancer Report 2014, posee el cuarto puesto en incidencia y mortalidad, se calcula que en 2018 se diagnosticaron unos 570.000 nuevos casos, suponiendo un 6.6% de los cánceres en mujeres y se registraron un total de 311.365 muertes siendo las poblaciones de regiones menos desarrolladas, incluidas en este grupo América Central y el Caribe, las más afectadas.
Su incidencia entre las mujeres de 20-54 años, en América Latina, es de 1: 1000 mujeres por año. Costa Rica presenta una incidencia de 20.2/1 00.000 mujeres, lo cual nos coloca entre los países de riesgo intermedio. En Costa Rica, para 2014, el cáncer de cérvix ocupaba el tercer lugar en incidencia, siendo más frecuente en las provincias de San José, Alajuela y Heredia, y el cuarto puesto en mortalidad para 2015, siendo Cartago y Alajuela las provincias más afectadas, según el Registro Nacional de Tumores (RNT) y el Instituto Nacional de Estadística y Censos (INEC).
FACTORES DE RIESGO
Los factores que pueden afectar el riesgo de cáncer de mama incluyen:
Al igual que con otras enfermedades crónicas, las tasas de incidencia y mortalidad del cáncer cervicouterino aumentan con la edad y a pesar de esto la mayor carga absoluta del cáncer cervicouterino recae sobre las mujeres de mediana edad. El cáncer cervicouterino representa uno de los pocos cánceres comunes en los cuales se ha identificado un agente causal específico.
La infección crónica del VPH es la causa fundamental en más del 99% de los casos de cáncer de cérvix. Además del VPH-16 y el VPH-18, los estudios internacionales recientes han ampliado la lista de los virus oncógenos para incluir los tipos 31, 33, 35, 45, 51, 52, 58 y 59. A nivel mundial, se ha registrado la prevalencia del VPH en 99,7 por ciento de los carcinomas cervicouterinos, y los tipos oncógenos 16 y 18 son los que se detectan con mayor frecuencia. Se consideran factores de riesgo todos aquellos relacionados con la adquisición de la infección.
Hay otros cánceres relacionados con la infección crónica por VPH como el cáncer de vulva (46%), vagina (70%), anal (88%), pene (50%) y orofaringe (26-50% dependiendo de la región geográfica).
El VPH es la infección de transmisión sexual más común y la mayoría de la población sexualmente activa entra en contacto con el virus a lo largo de su vida. La infección es asintomática así que muchos de los infectados lo desconocen y por lo tanto lo pueden transmitir. Hasta un 90% de las infecciones por VPH se eliminan sin tratamiento durante los primeros dos años y sólo aquellas que se cronifican pueden dar lugar a lesiones precancerosas que progresen a cáncer invasivo.
Se han evaluado agentes ambientales tales como el humo del tabaco, los anticonceptivos hormonales, el régimen alimentario y diversos microorganismos infecciosos como posibles cofactores del VPH en la carcinogénesis cervical. Estudios epidemiológicos bien controlados han demostrado que las pacientes con cáncer cervicouterino positivo al VPH tienen el doble de probabilidades de haber sido fumadoras que las testigos positivas al VPH. Además, algunos estudios recientes en mujeres positivas al VPH han indicado que el riesgo de cáncer cervicouterino es mayor en las mujeres que han usado anticonceptivos orales durante más de 10 años.
- Edad temprana de inicio de las relaciones sexuales
- Promiscuidad sexual o parejas de alto riesgo
- Inmunosupresión (trasplantadas, pacientes con enfermedades autoinmunes en tratamiento con esteroides, VIH, etc…)
- Antecedentes de coinfección por enfermedad de transmisión sexual.
- Uso de píldora anticonceptiva, porque suele llevar asociado no usar métodos barrera.
- Falta de adherencia al programa de cribado poblacional
- Tabaquismo, duplican su riesgo respecto a las no fumadoras.
- Multiparidad y primer embarazo a una edad temprana
- Tipo de infección por VPH, debido al potencial oncogénico de cada subtipo.

En los estadios más tempranos la enfermedad es frecuentemente asintomática. Los síntomas más precoces incluyen:
SÍNTOMAS: Sangrado genital anómalo (irregular/intermitente), Sangrado tras relaciones sexuales (coitorragia) o durante el examen ginecológico, Flujo maloliente, es muy inespecífico, pero puede ser indicativo de vaginitis o cervicitis, Dolor pélvico o lumbar, Molestias al orinar (disuria) o tenesmo rectal, Sangrado ginecológico tras la menopausia, Dolor durante las relaciones sexuales (dispareunia).
DIAGNÓSTICO: La citología mediante técnica de Papanicolaou tiene una baja sensibilidad para el diagnóstico de lesiones de alto grado, pero compensa con una alta especificidad. La combinación de la detección molecular del virus del papiloma humano (VPH) y la citología alcanza una sensibilidad para detectar estas lesiones de hasta el 96%. En un escenario de vacunación como el que se está implantando para esta patología.
La prueba de Papanicolaou ha reducido la tasa de incidencia del cáncer de cuello uterino en un 60%-90% y la tasa de mortalidad en un 90%. Más recientemente, se ha introducido una prueba de detección del ADN del VPH que tiene una mayor sensibilidad para la NIC de alto grado respecto a la prueba de Papanicolaou y se ha demostrado que proporciona un 60%-70% más de protección contra el cáncer invasivo en comparación con esta última.
HERRAMIENTAS DIAGNÓSTICAS
Exploración física y ginecológica: Se realiza un examen visual del cérvix con espéculo. Aquellas lesiones visibles con esta técnica incluyen ulceraciones, tumores exofíticos en el exocérvix e infiltración del endocérvix.
Citología cervical (Papanicolaou): Es el principal método de cribado poblacional. Identifica células anormales. Sensibilidad baja pero alta especificidad.
Prueba de VPH: Prueba de alta sensibilidad y especificidad.
Colposcopia: Se realiza cuando alguna de las pruebas de cribado resulta positiva o si existe sospecha clínica. Permite ver con mayor detalle la morfología de lesiones sospechosas y en el mismo acto tomar biopsias.
Biopsia cervical: Consiste en la toma de un pequeño fragmento de la lesión sospechosa para corroborar el diagnóstico de sospecha.
Pruebas de imagen:
– Radiografía de tórax.
– Cistoscopia y/o rectosigmoidoscopia: consiste en realizar una visualización directa de vejiga y recto respectivamente ante la sospecha de infiltración por el tumor.
– Urografía: permite valorar las vías urinarias ante la sospecha de enfermedad localmente avanzada.
– Ecografía Transvaginal.
– Tomografía Computarizada (TC): se puede utilizar en lugar de la radiografía de tórax y urografía para el estadiaje y también resulta de utilidad para la valoración de la afectación ganglionar.
– Resonancia Magnética: prueba de gran utilidad para la estadificación local de la enfermedad determinando el tamaño del tumor, la invasión de tejidos adyacentes y la afectación ganglionar.
Tomografía por emisión de positrones (PET): Este examen por imágenes de medicina nuclear utiliza una pequeña cantidad de material radiactivo para ayudar a determinar el grado de diseminación del cáncer cervical.

El tratamiento depende del diagnóstico, del tamaño, localización y estadio del tumor, así como de su estado general de salud y su estado físico. Según la extensión del cáncer y de la evaluación del riesgo, el tratamiento puede consistir en una o más terapias:
CIRUGÍA: El programa convencional para administrar radiación a todo el seno es de 5 días a la semana (de lunes a viernes) por 6 a 7 semanas. Otra opción es radioterapia hipo fraccionada en la que también se administra radiación a todo el seno, pero en dosis diarias más elevadas (de lunes a viernes) utilizando menos tratamientos (por lo general durante solo 3 a 4 semanas).
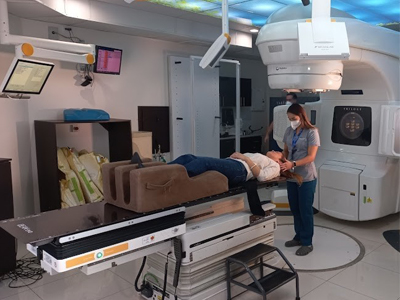
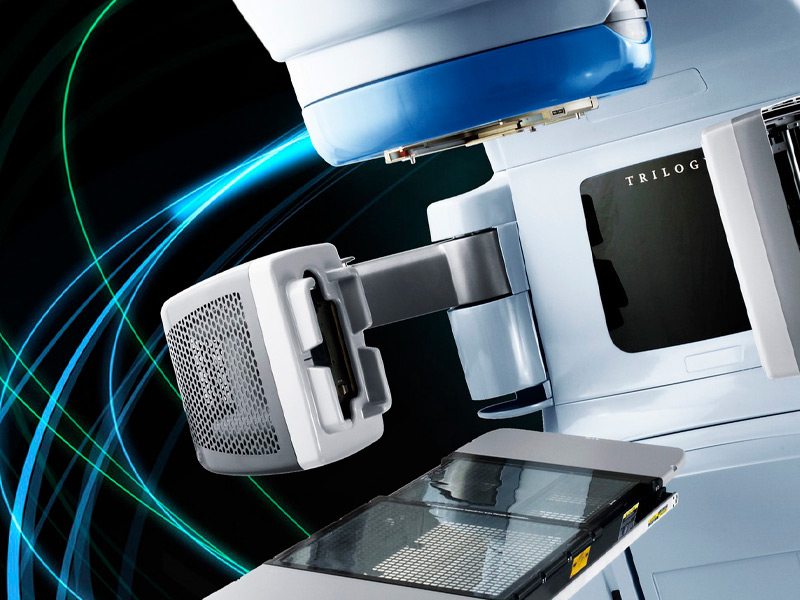
RADIOTERAPIA: La radioterapia podría ser administrada después de la cirugía o en lugar de la cirugía, y es el tratamiento predilecto durante cualquier etapa de la enfermedad, con excepción de las etapas más tempranas. También se utiliza para tratar a algunas pacientes con cáncer de cuello uterino localmente avanzado y también se puede utilizar para tratar algunos síntomas de la enfermedad metastásica, esto como terapia neoadyuvante o adyuvante dependiendo del caso. Es un tratamiento que se administra de forma ambulatoria 5 días a la semana, durante 5 semanas aproximadamente. La administración del tratamiento de radioterapia dura unos pocos minutos, y no es doloroso.
En la actualidad existen técnicas avanzadas de tratamiento con radioterapia externa muy sofisticadas que permiten administrar altas dosis de radiación sobre la zona de tratamiento minimizando la dosis de radiación sobre los órganos sanos que rodean el tumor y demostrando que la sobrevida global y el periodo libre de enfermedad en este tipo de patología se favorecen con la aplicación de estas técnicas.
Actualmente la Clínica de Radioterapia Siglo XXI cuenta con estas tecnologías y la experiencia para tratar este tipo de patologías, garantizando la protección de órganos y tejidos circundantes, con disminución en las toxicidades a nivel del tracto urinario y del tracto gastrointestinal brindando así una mayor calidad de vida para la paciente. Dichas técnicas son:
* IMRT (radioterapia de intensidad modulada): Permite variar la dosis de RT y la intensidad durante la terapia. Es una tecnología a través de un sistema computarizado que permite administrar dosis de radiación precisas a un tumor o a áreas específicas dentro de un tumor y reducir las dosis en tejidos sanos.
* VMAT (Arcoterapia volumétrica) : Esta técnica emplea una máquina controlada por una computadora que se mueve alrededor del paciente a medida que emite la radiación y acorta de forma muy importante los tiempos de irradiación, contribuyendo a aumentar aún más la seguridad del tratamiento y mejorando el confort del paciente.
* IGRT: Permite la administración de dosis más altas de radioterapia mediante la utilización de técnicas de imagen avanzada como la resonancia magnética con espectroscopia o un escáner de imágenes integrado. Este adelanto le permite al médico tomar fotografías del área justo antes de administrar la radiación para hacer ajustes menores en la dirección de los rayos ayudando a administrar la radiación incluso de forma más precisa.
QUIMIOTERAPIA: El uso de la radioterapia como parte del tratamiento de las neoplasias malignas de recto está cada vez más extendido. En el cáncer primario de recto localmente avanzado, varios estudios han demostrado su eficacia, con una disminución de la recidiva local y un aumento de la supervivencia libre de enfermedad, tanto en su administración preoperatoria como postoperatoria. Desarrollos emergentes como la radioterapia con intensidad modulada (IMRT), radioterapia guiada por imagen (IGRT) y radioterapia estereotáctica (SBRT) están siendo evaluados. Estas técnicas ofrecen la posibilidad de dar mayor radioterapia sin involucrar tejido normal o sano.