Cervix Cancer

What is Cervix cancer?
Cervical cancer begins when healthy cells on its surface start to divide uncontrollably. These changes cause abnormalities that are not necessarily cancerous but are the first steps that can lead to the development of cancer.
Cervical cancer is one of the most common cancers among women worldwide, ranking fourth in both incidence and mortality.
There are currently specialized radiotherapy techniques that contribute to disease control. Learn more in the following section
RISK FACTOR'S
Factors that may affect breast cancer risk include:
As with other chronic diseases, the incidence and mortality rates of cervical cancer increase with age; nevertheless, the greatest absolute burden of cervical cancer falls on middle-aged women.
“Cervical cancer is one of the few common cancers in which a specific causal agent has been identified.”
Chronic HPV infection is the primary cause in more than 99% of cervical cancer cases. In addition to HPV-16 and HPV-18, recent international studies have expanded the list of oncogenic viruses to include types 31, 33, 35, 45, 51, 52, 58, and 59.
Worldwide, HPV prevalence has been recorded in 99.7 percent of cervical carcinomas, with oncogenic types 16 and 18 being the most frequently detected. All factors related to acquiring the infection are considered risk factors.
HPV is the most common sexually transmitted infection, and the majority of sexually active people come into contact with the virus at some point in their lives.
Environmental agents such as tobacco smoke, hormonal contraceptives, diet, and various infectious microorganisms have been evaluated as possible cofactors of HPV in cervical carcinogenesis.
Well-controlled epidemiological studies have shown that patients with HPV-positive cervical cancer are twice as likely to have been smokers compared to HPV-positive controls. Additionally, some recent studies in HPV-positive women have indicated that the risk of cervical cancer is higher in those who have used oral contraceptives for more than 10 years.
Factors to consider:
- Early age of initiation of sexual relations
- High-risk partners
- Immunosuppression (transplant patients, patients with autoimmune diseases being treated with steroids, HIV, etc…)
- History of coinfection with a sexually transmitted disease.
- Use of the contraceptive pill, because it is usually associated with not using barrier methods.
- Smoking doubles their risk compared to non-smokers.
- Multiparity and first pregnancy at a young age
- Type of HPV infection, due to the oncogenic potential of each subtype.

In the earliest stages the disease is frequently asymptomatic. The earliest symptoms include:
SYMPTOMS:
Abnormal genital bleeding (irregular/intermittent), Bleeding after sexual intercourse (coitorrhagia) or during gynecological examination, Smelly discharge, is very nonspecific, but may be indicative of vaginitis or cervicitis, Pelvic or lower back pain, Discomfort when urinating (dysuria) or Rectal tenesmus, Gynecological bleeding after menopause, Pain during sexual relations (dyspareunia).
DIAGNOSIS:
Cytology using the Papanicolaou technique has low sensitivity for diagnosing high-grade lesions but compensates with high specificity.
The combination of molecular detection of human papillomavirus (HPV) and cytology achieves a sensitivity of up to 96% for detecting these lesions.
The Papanicolaou test has reduced the incidence rate of cervical cancer by 60%–90% and the mortality rate by 90%.
DIAGNOSTIC TOOLS
Physical and gynecological examination:
A visual examination of the cervix is performed using a speculum. Lesions visible with this technique include ulcerations, exophytic tumors on the exocervix, and infiltration of the endocervix.
Cervical cytology (Papanicolaou):
It is the main population screening method. It identifies abnormal cells. It has low sensitivity but high specificity.
HPV test:
A test with high sensitivity and specificity.
Colposcopy:
It is performed when any of the screening tests are positive or if there is clinical suspicion. It allows for a more detailed view of the morphology of suspicious lesions and enables biopsies to be taken during the same procedure.
Cervical biopsy:
It involves taking a small sample of the suspicious lesion to confirm the suspected diagnosis.
Image tests:
– Cystoscopy and/or rectosigmoidoscopy: It consists of performing a direct visualization of the bladder and rectum respectively in case of suspicion of infiltration by the tumor.
– Urography: allows evaluation of the urinary tract in the event of suspicion of locally advanced disease.
– Transvaginal Ultrasound.
– Computed Tomography (CT): It can be used instead of chest x-ray and urography for staging and is also useful for assessing lymph node involvement.
– Magnetic resonance: very useful test for local staging of the disease by determining tumor size, invasion of adjacent tissues and lymph node involvement.
Positron emission tomography (PET): This nuclear medicine imaging test uses a small amount of radioactive material to help determine how much cervical cancer has spread.

Treatment depends on the diagnosis, the size, location and stage of the tumor, as well as your general health and physical condition. Depending on the extent of the cancer and risk assessment, treatment may consist of one or more therapies:
SURGERY:
The conventional schedule for delivering radiation to the whole breast is 5 days a week (Monday through Friday) for 6 to 7 weeks. Another option is hypofractionated radiation therapy in which radiation is also given to the entire breast, but in higher daily doses (Monday through Friday) using fewer treatments (usually for only 3 to 4 weeks).
RADIOTHERAPY:
Radiotherapy may be administered after surgery or instead of surgery, and it is the preferred treatment at any stage of the disease, except for the earliest stages.
It is also used to treat some patients with locally advanced cervical cancer and can be used to manage certain symptoms of metastatic disease, serving as neoadjuvant or adjuvant therapy depending on the case.
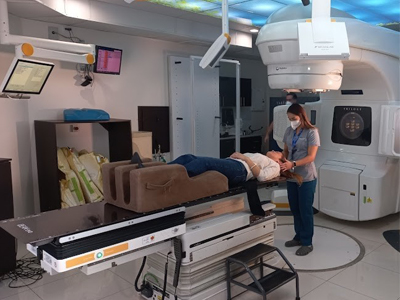
It is a treatment administered on an outpatient basis, 5 days a week, for approximately 5 weeks. The administration of radiotherapy treatment lasts only a few minutes and is not painful.
Currently, there are very sophisticated advanced treatment techniques with external radiotherapy that allow high doses of radiation to be administered to the treatment area, minimizing the radiation dose to the healthy organs surrounding the tumor and demonstrating that the overall survival and the disease-free period In this type of pathology, the application of these techniques is favored.
Currently, the Centro Médico de Radioterapia Siglo XXI has these technologies and the expertise to treat these types of conditions, ensuring the protection of surrounding organs and tissues, reducing toxicities in the urinary and gastrointestinal tracts, thereby providing a higher quality of life for the patient. These techniques include:
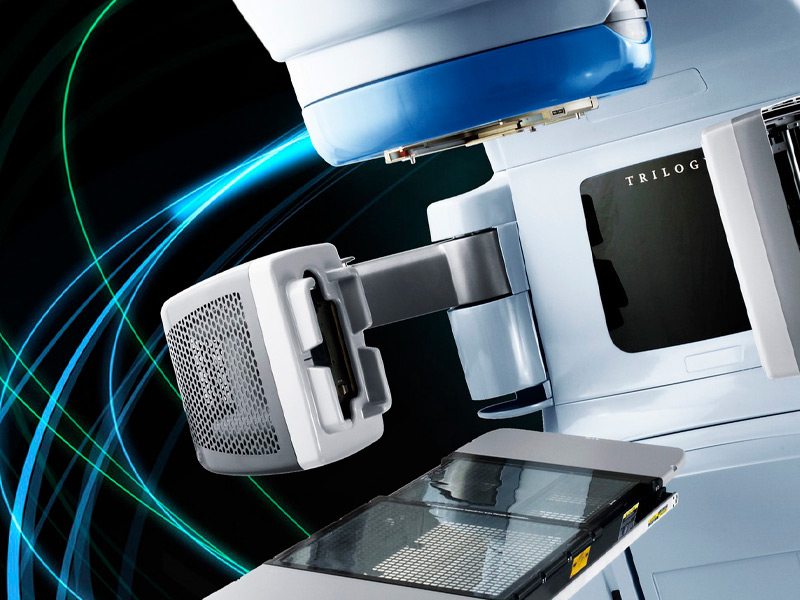
Intensity Modulated Radiotherapy IMRT
It allows variation of the radiotherapy dose and intensity during treatment. This computerized technology enables the delivery of precise radiation doses to a tumor or specific areas within a tumor while reducing doses to healthy tissues.
* IGRT:
It allows the delivery of higher doses of radiotherapy through the use of advanced imaging techniques such as magnetic resonance spectroscopy or an integrated imaging scanner. This advancement enables the physician to take images of the area just before administering radiation to make minor adjustments in the beam direction, helping to deliver radiation even more precisely.
CHEMOTHERAPY:
The use of radiotherapy as part of the treatment of rectal malignancies is increasingly widespread. In locally advanced primary rectal cancer, several studies have demonstrated its effectiveness, with a decrease in local recurrence and an increase in disease-free survival, both in its preoperative and postoperative administration. Emerging developments such as intensity-modulated radiation therapy (IMRT), image-guided radiation therapy (IGRT), and stereotactic radiation therapy (SBRT) are being evaluated. These techniques offer the possibility of providing greater radiotherapy without involving normal or healthy tissue.