Cranial Stereotaxic Radiosurgery
Stereotactic Radiosurgery (SRS) es una forma de radioterapia sumamente precisa, inicialmente desarrollada para tratar tumores pequeños y anomalías funcionales del cerebro.
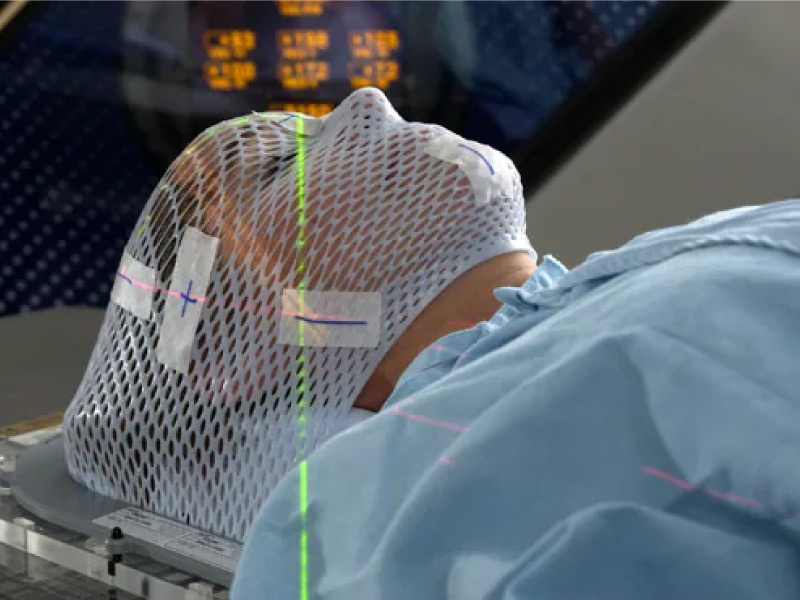
A pesar de su nombre y en comparación con la radioterapia tradicional, la SRS es un procedimiento no quirúrgico que entrega radiación sumamente enfocada, en dosis mucho más altas y en solamente uno o unos pocos tratamientos. Este tratamiento es posible gracias al desarrollo de tecnologías altamente avanzadas que permiten la entrega de dosis máximas de radiación dentro del blanco, mientras se reducen al máximo la dosis que recibe el tejido sano circundante, destruyendo el tumor y logrando un máximo control local.
La SRS se usa para tratar muchos tipos de patologías cerebrales que incluyen: Tumores benignos o malignos; primarios y metastáticos ya sean simples o múltiples. Además, tumores residuales después de la cirugía; tumores intracraneales, orbitales y en la base del cráneo; así como malformaciones arteriovenosas (MAV) y otras condiciones como la neuralgia del trigémino, etc.
Who participates in this procedure and who manages the equipment?
The treatment team is made up of several specialized medical professionals, typically radiation oncologists, a medical physicist, imaging scientists, a dosimetrist, and a radiation therapy nurse.
- The radiation oncologist and in some cases, a neurosurgeon lead the treatment team and monitor the treatment; They outline the target areas to be treated, decide the appropriate dose of radiation, approve the treatment plan, and interpret the results of the radiosurgical procedures.
- An imaging specialist interprets images that identify target areas to be treated in the brain or body.
- The medical radiation physicist ensures the delivery of the precise dose of radiation.
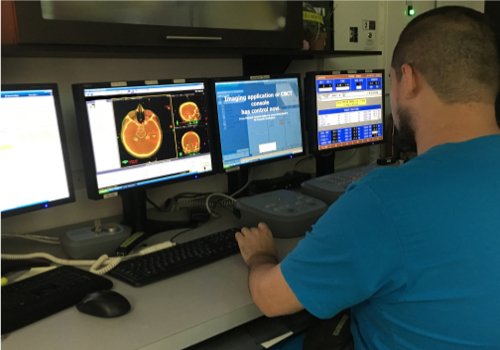
- The physicist, or a dosimetrist under the physicist's supervision, uses special computer software to prepare a treatment plan; Calculates exposures and beam configuration to treat areas according to the prescribed dose.
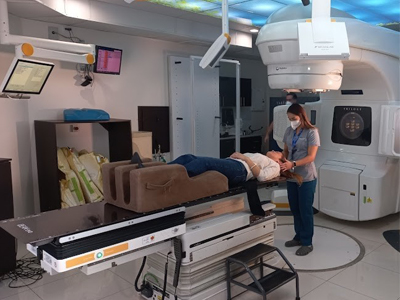
- A highly trained imaging specialist positions the patient on the treatment table and operates the machine from an adjacent protected area.
- The imaging doctor can observe the patient through a window or closed-circuit television and can communicate with the patient throughout the procedure. In the case of the gamma knife, the neurosurgeon and/or radiation oncologist can help position the patient for treatment and the imaging doctor can operate the machine.
- The radiation therapy nurse evaluates the patient, provides the patient with information about the treatment, monitors the patient during treatment, and helps answer questions after treatment.
- A neurologist or neurooncologist may participate with the radiation oncologist and neurosurgeon in the multidisciplinary team that considers various treatment options for individual cases and helps decide who may benefit from radiosurgery for brain lesions.
Special preparations needed for the procedure
They are generally performed on an outpatient basis. However, it's best to prepare to spend anywhere from half a day or more in the imaging department. You will be informed if you will need to have someone accompany you and drive you home after the procedure.
You may be told not to eat or drink anything after midnight before treatment. Ask your doctor if you should continue taking your regular medications on the day of treatment and if you should bring your medications with you to the procedure.
Tell your doctor if any of the following apply to you:
- You are taking oral medications or use insulin to control diabetes.
- You have an allergy to intravenous contrast media or iodine.
- You have a pacemaker, artificial heart valve, defibrillator, brain aneurysm clamps, implantable chemotherapy pumps or ports, neurostimulators, eye or ear implants, stents, coils or filters.
- Suffers from claustrophobia
What does it feel like during and after the procedure?
Radiosurgery treatments are similar to taking x-rays. X-rays are generally not seen, felt, or heard, with the exception of patients receiving brain treatment, in which case they may see lights while the machine is on, even with their eyes. closed. The treatment itself does not cause any pain or discomfort. If you have pain for other reasons, such as back pain or discomfort from the headgear or immobilization device, tell the medical or nursing staff.
1- En la mayoría de los casos, los pacientes que se han sometido a la radiocirugía y SRS pueden retomar tomas sus actividades normales dentro de uno o dos días.
2- Los efectos secundarios de la radioterapia pueden darse como resultado del tratamiento mismo así como del leve daño ocasionado por el tratamiento a las células sanas en el área del tratamiento.
3- El número y la severidad de los efectos secundarios que usted experimenta dependen del tipo de radiación y la dosificación que recibe y la parte del cuerpo sometiéndose a tratamiento. Debe hablar con el medico y la enfermera acerca de cualesquiera efectos secundarios que experimenta para que puedan ayudarle a controlarlos.
4- La radioterapia puede causar efectos secundarios tempranos durante o inmediatamente después del tratamiento, y normalmente desaparecen a las pocas semanas. Los efectos secundarios tardíos pueden ocurrir meses o años más tarde. Los efectos secundarios tempranos comunes de la radioterapia incluyen cansancio o fatiga y problemas en la piel. La piel en el área de tratamiento puede ponerse más sensible, roja, irritada o hinchada.

Depending on the area undergoing treatment, other early side effects may include:
- Hair loss in the treatment area
- Mouth problems and difficulty swallowing
- Problems with eating and digestion
- Nausea and vomiting
- Headaches
- Tenderness and swelling in the treatment area
Delayed side effects, which are rare, occur months or years after treatment and are often permanent. They include:
- Brain changes
- Changes in the spine
- Changes in the situation
- Lymphedema
- Changes in the mouth
Después de radioterapia o radiocirugía usted debe someterse exámenes regulares y chequeos de control.
When using techniques such as SRS the goal is to maximize the cancer-destroying abilities of radiotherapy, while minimizing its effects on healthy tissues and organs, thereby avoiding the side effects of the treatment itself.