4D Motion Compensatory Radiotherapy

4D Motion Compensatory Radiotherapy, also known as “Fourth Dimensional Radiotherapy”, technology used by Varian's RPM system.
This modality allows monitoring, while taking computed tomography images, in the various phases of the respiratory cycle and in this way doctors can choose the most appropriate moment in the patient's cycle to activate the treatment.
The equipment allows us to optimize the previous time in the application of the treatments that are currently carried out, since it has the necessary technology to protect the organs around the area to be irradiated, and also modulate the intensity through the integrated multi-leaf collimator (MLC) system. )
Who participates in this procedure and who manages the equipment?
Most medical centers have a team of staff specially trained in administering IMRT. The radiation oncologist, medical physicist, dosimetrist, imaging scientists, and radiotherapy nursing staff participate in this team.
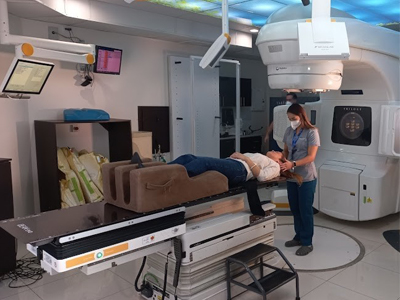
The radiation oncologist, a specially trained doctor, first consults with the patient to determine if radiation therapy with IMRT is the most appropriate treatment. After obtaining informed consent, an individualized course of treatment is established. A radiophysicist, who has specialized training in the field of radiation oncology physics, ensures that the linear accelerator delivers the precise dose of radiation and that the computerized dose calculations are correct. A dosimetrist works with the medical radiophysicist to calculate IMRT exposures and the beam configurations needed to deliver the dose prescribed by the radiation oncologist. The final treatment plan is verified by the medical physicist, with measurements on the machine, before being administered to the patient. A highly specialized imaging specialist places the patient on the treatment table and operates the machine. The radiation oncology nurse assesses the patient on the treatment table and provides additional information about the treatment and possible adverse reactions. The radiation oncology nurse, in collaboration with the doctor, also helps monitor reactions or side effects that may occur.
- The imaging specialist operates the equipment from a nearby area protected from radiation. The therapist can communicate with the patient throughout the procedure, and may observe the patient through a window or via closed-circuit television.
- A neurologist or neurooncologist may participate with the radiation oncologist and neurosurgeon in the multidisciplinary team that considers various treatment options for individual cases and helps decide who may benefit from radiosurgery for brain lesions.
Special preparations needed for the procedure
Before treatment planning, a physical examination is done and the medical history is reviewed. Next, there is a treatment simulation session, in which a CT scan is done that allows the radiation oncologist to specify the three-dimensional shape of the tumor and normal tissues. In most cases, a treatment preparation session may be necessary to mold a special device that helps the patient maintain the exact treatment position. Sometimes, prior to the simulation, the patient is instructed to follow certain bowel and bladder preparation regimens. The dosimetrist and physician use the CT information to design the IMRT beams that, under specifications from the radiation oncologist, will be used during treatment. Sometimes intravenous contrast agents are injected during the CT scan to help better define the tumor. Occasionally, other diagnostic procedures, such as positron emission tomography (PET) and magnetic resonance imaging (MRI), may be necessary for IMRT planning. These diagnostic images can be combined with planning CT and help the radiation oncologist determine the exact location of the tumor to be treated. In some cases it is necessary to insert dense radio markers within the target area for more precise positioning. Typically, IMRT sessions begin about a week after the simulation. Before treatment, the patient's skin may be marked or tattooed with a colored ink, which will help align the equipment with the area to be treated.
What does it feel like during and after the procedure?
As with other external beam radiation therapy treatments, there is no expected pain during the treatment itself. However, it is possible to stop the machine if you experience discomfort due to the treatment position or positioning devices. As treatment progresses, some patients may experience certain treatment-related side effects. The nature of the side effects depends on which normal tissue structures are being irradiated. The radiation oncologist and nurse will talk to you about this and help you if you have side effects.
Side effects of radiation therapy include problems that occur as a result of the treatment itself as well as damage done by the treatment to healthy cells in the treatment area.
The number and severity of side effects you experience depend on the type of radiation and dosage you receive and the part of the body undergoing treatment. You should talk to your doctor and nurse about any side effects you experience so they can help you manage them.
Radiation therapy can cause early and delayed side effects. Early side effects occur during or immediately after treatment and usually disappear within a few weeks. Common early side effects of radiation therapy include tiredness or fatigue and skin problems. The skin in the treatment area may become more sensitive, red, irritated or swollen. Other skin changes include dryness, itching, peeling, and blistering.
Depending on the area undergoing treatment, other early side effects may include:
- Hair loss in the treatment area
- Mouth problems and difficulty swallowing
- Problems with eating and digestion
- Diarrhea
- Nausea and vomiting
- Headaches
- Tenderness and swelling in the treatment area
- Urinary and bladder changes
Delayed side effects, which are rare, occur months or years after treatment and are often permanent. They include:
- Brain changes
- Changes in the spine
- Lung changes
- Liver changes
- Changes in the colon and rectum
- Infertility
- Changes in the situation
- Lymphedema
- Changes in the mouth
- Secondary cancer
There is a small risk of developing cancer from radiation therapy. After radiation therapy for cancer, you should undergo regular examination by your radiation oncologist to detect recurring and new cancers.
Using techniques such as IMRT, radiation oncologists are maximizing the cancer-destroying abilities of radiation therapy while minimizing its effect on healthy tissues and organs and the side effects of the treatment itself.