Breast Cancer and its Treatment
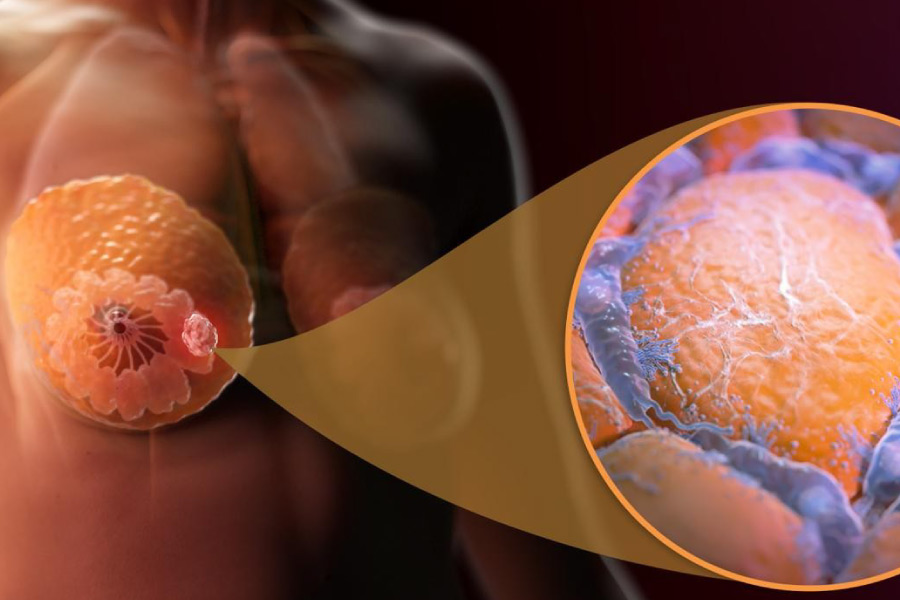
What is breast cancer?
EPIDEMIOLOGY
Breast cancer is the leading cause of death in women in developing countries and the second cause of death in developed countries, second only to lung cancer. Compared with international data, an incidence of 30-39.9 cases/100 thousand inhabitants is documented in Costa Rica and in Latin Americans 4.1, this being lower in relation to the incidence of cases in countries in North America, Australia and North-Western Europe where the incidence is around 78-90/100 thousand inhabitants.
RISK FACTOR'S
Factors that may affect breast cancer risk include:

RISK FACTOR'S: Factors that may affect breast cancer risk include:
AGE:The most important risk factor for breast cancer is age. Most breast cancers occur in women > 50.
FAMILY BACKGROUND: Having a first-degree relative (mother, sister, daughter) with breast cancer doubles or triples the risk of developing it, but the risk in more distant relatives increases only slightly.
GENE MUTATION FOR BREAST CANCER: About 5 to 10% of women with breast cancer carry a mutation in 1 of 2 known breast cancer genes, BRCA1 or BRCA2. If these women's relatives also carry the mutation, they have a 50 to 85% lifetime risk of developing breast cancer.
PERSONAL HISTORY: Having had invasive breast cancer increases your risk. The risk of developing cancer in the contralateral breast after mastectomy is 0.5 to 1%/year of follow-up.
GYNECOLOGICAL HISTORY: Early menarche, late menopause, or a late first pregnancy increase the risk.
BREAST CHANGES: A history of an injury that required a biopsy slightly increases the risk. Benign lesions that may slightly increase the risk of invasive breast cancer are complex fibroadenoma, moderate or florid hyperplasia (without atypia), sclerosing adenosis, and papilloma. An increase in breast density on a screening mammogram is associated with an increased risk of breast cancer.
USE OF ORAL CONTRACEPTIVES: Oral contraceptives increase the risk very slightly (about 5 more cases per 100,000 women). The risk increases primarily during the years of contraceptive use and decreases slowly during the 10 years following discontinuation.
Early detection
Breast cancer is a major health problem worldwide. Despite diagnostic and therapeutic advances, its prognosis continues to depend mainly on the extent of the disease at the time of detection. Hence, getting an early diagnosis remains the best way to improve your chances of cure.
Mammography has been proven to be the most effective diagnostic test; it reduces mortality from breast cancer.

SYMPTOMS: A lump or thickening in the breast that feels different from the tissue around it. A palpable nodule in the breast is the most common sign, generally painless. Change in size, shape or appearance of a breast. Changes in the skin over the breast, such as dimpling.
Recent nipple inversion scaly, peeling, crusting, and peeling of the pigmented area of skin surrounding the nipple (areola) or breast skin, Redness or small holes in the skin over your breast , like the peel of an orange.
DIAGNOSIS: When there is a suspicion of breast cancer either through physical examination (both by the patient and a doctor) or by a routine mammogram, a study is initiated to confirm or rule out that suspicion. Imaging tests will guide the diagnosis, but a certain diagnosis of breast cancer always requires confirmation with a biopsy.
WITHIN THE TESTS ARE
SELF-EXPLORATION: It has not been proven effective in reducing the mortality of the disease.
MAMMOGRAPHS: They are X-ray images that detect abnormal areas in the breast. They do not have a 100% reliability so they may give suspicious images that are ultimately not malignant (false positives) or fail to diagnose a malignant tumor (false negatives).
ULTRASOUNDS: Technique that uses ultrasound to produce an image and can distinguish cystic lesions (fluid-filled, normally non-tumorous) from solid lesions (more suspicious). Many times this technique complements mammography. Ultrasound can also assess the status of the lymph nodes in the armpit, which are the first site of spread of breast cancer.
NUCLEAR MAGNETIC RESONANCE: It is a radiological examination that uses the action of an electromagnetic field to obtain images. It may be necessary in women with dense breast tissue, women with a BRCA gene mutation or women wearing silicone prostheses.
If breast cancer is suspected, the next step is to take a tissue sample for analysis.
BIOPSY: It consists of extracting a sample of tissue from the suspicious area to analyze it microscopically and determine its benign or malignant characteristics, as well as the type of tumor cells, their degree of aggressiveness and some other parameter of interest. when making decisions about treatment.
The biopsy can be done by direct palpation or guided by ultrasound. This can be done with a fine needle (FNAB) or with a thick needle (CNA) to obtain a greater amount of tissue. Sometimes a biopsy may be necessary in the operating room.
TREATMENT
Your doctor determines breast cancer treatment options based on the type of breast cancer, its stage, grade, size, and whether the cancer cells are sensitive to hormones. Treatment will depend on the stage at the time of diagnosis, whether it is ER/PR positive or not, HER2 positive or not. Surgery (stage I, II, IIIA to IIIC), is a pillar of breast cancer treatment. There are two (2) options:
- Breast-conserving surgery
- Modified radical mastectomy with dissection of axillary lymph node levels 1 and 2 with or without breast reconstruction.

The Sentinel node, the node where the nodal metastasis from the primary tumor is first discovered, has come to replace routine axillary nodal dissection, thereby reducing the morbidity that this entails; such as edema of the upper limb, neuropathies. Sentinel lymph node biopsy is a standard procedure and cannot be replaced by imaging studies such as MRI or CT scan.
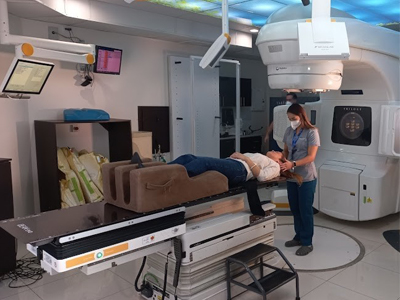
Radiotherapy: Used post-surgery in breast conservation (since recurrence is >20%) or in cancer with high risk of local recurrence. Its purpose is to eradicate residual disease. Radiotherapy after breast-conserving surgery significantly reduces the incidence of local recurrences in the breast and regional nodes and may improve the overall survival rate.
The Siglo XXI Radiotherapy Medical Center is the only center in the country that offers high-precision treatments that allow partial or high-dose regimens to be applied that better preserve healthy tissue and in a shorter amount of time.
Below are the details of some of these treatments:
RADIATION TO THE WHOLE BREAST: The conventional schedule for delivering radiation to the whole breast is 5 days a week (Monday through Friday) for 6 to 7 weeks. Another option is hypofractionated radiation therapy in which radiation is also given to the entire breast, but in higher daily doses (Monday through Friday) using fewer treatments (usually for only 3 to 4 weeks).
PARTIAL BREAST IRRADIATION: Intensity-modulated radiation therapy (IMRT): IMRT delivers powerful doses to certain parts of the tumor bed and helps reduce damage to adjacent normal body tissues.
4D RADIOTHERAPY: It is a technique that takes into account the movement of the tumor not only during treatment but also during planning. To do this, the patient's image acquisition system not only takes the images at a given moment, but a series of images are obtained with the treatment area with the different positions it can adopt. It takes into account the patient's respiratory cycles which are considered in treatment planning, in this way the equipment and the dose are calibrated to apply the treatment doses in the most optimal phases of the respiratory cycle.
IMAGE GUIDED RADIOTHERAPY (IGRT): This technique uses high-resolution three-dimensional images to locate the precise location of tumors, adjust the patient's position for maximum precision, and deliver radiation therapy. This allows the area to be treated to be determined in the most precise way and the areas surrounding the treatment area to be maximally protected. This technology places the patient at the exact point that should be treated to almost exclusively irradiate the injury and not damage important organs such as the heart or lungs; technology that is not available in conventional radiotherapy systems.
RADIOSURGERY: High doses in few treatments (5 sessions). Despite its name and compared to traditional radiation therapy, it is a non-surgical procedure that delivers highly focused radiation at much higher doses and in only a few treatments in the case of breast cancer. The adjuvant treatment of breast cancer with external radiation therapy can currently be applied in 5 consecutive days based on the results of the phase III FAST-Forward study (Murray Brunt, 2020) and the Siglo XXI Radiotherapy Medical Center is the pioneer in apply this technique in Costa Rica.