Guided Image Radiotherapy
It allows
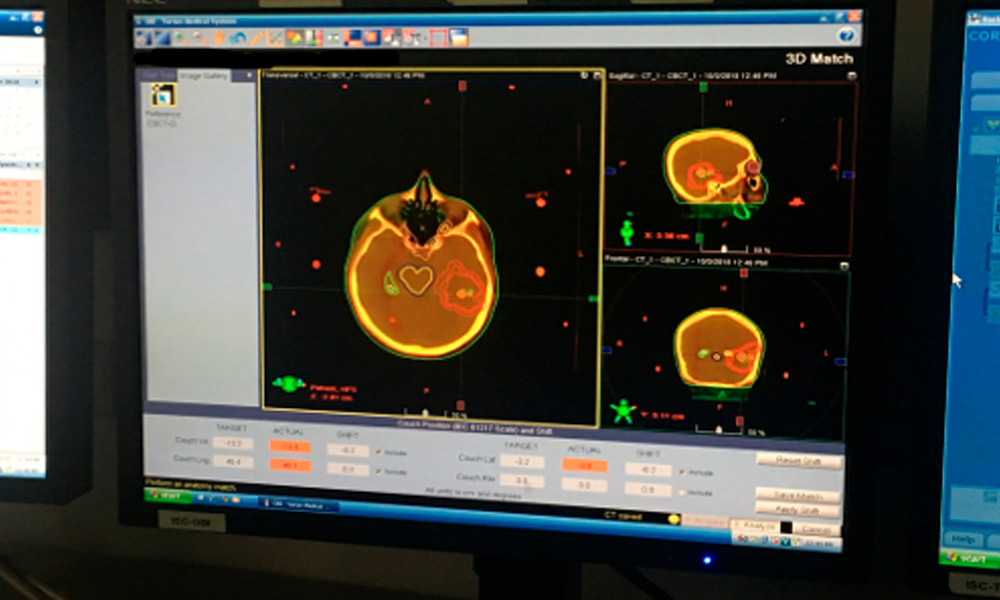
- Confirm and follow tumor movement at the time of treatment.
- Minimize the risk of side effects.
- Higher doses of radiation – ultimately leads to higher cure rates.
- Correct changes in the patient's anatomy: Gain or lose weight over 25 to 35 days.
- It allows daily positioning to be corrected, since tumors can move several centimeters when patients breathe during treatment.
Who participates in this procedure and who manages the equipment?
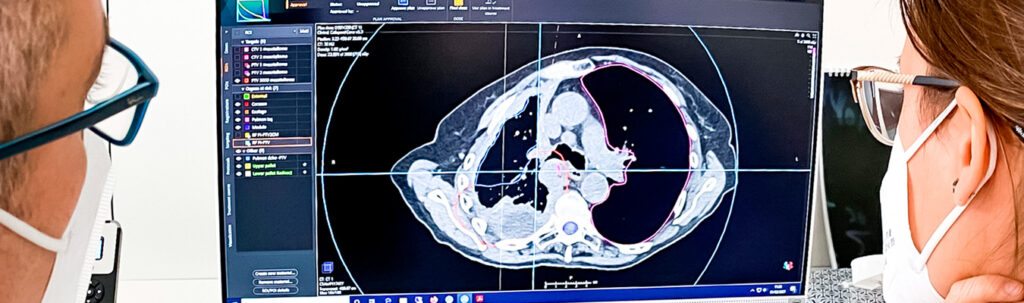
The delivery of radiation therapy requires a treatment team, including a radiation oncologist, medical physicist, dosimetrist, and imaging scientists. The radiation oncologist is a doctor who evaluates the patient and determines the appropriate therapy or combination of therapies and the type of IGRT. The doctor determines which area should be treated and the dosage to be delivered. In conjunction with the physical therapist and dosimetrist, the physician determines which techniques should be used to deliver the prescribed dosage. The physicist and dosimetrist then make detailed treatment calculations. Imaging scientists are specially trained technologists who acquire images and deliver daily treatments. The radiation oncology nurse evaluates the patient and provides additional information about treatment and possible adverse reactions. The radiation oncology nurse, in collaboration with the doctor, also helps monitor any reactions or side effects that may occur due to the treatment.
The equipment is operated by an imaging specialist, a highly trained technologist. The overall treatment plan is created and monitored by a radiation oncologist, a highly trained doctor who specializes in treating cancer with radiation therapy.
- Women should always tell their doctor or technologist if there is any possibility that they are pregnant or if they are breastfeeding their baby.
- See the Safety page for more details regarding pregnancy, breastfeeding, and imaging.
- Patients with pacemakers or loose metal in their bodies should inform the treatment team if MRI is being used for simulation or IGRT.
- For some IGRT procedures, fiducial markers or electromagnetic transponders may be placed inside the body, near or inside the tumor, to help the treatment team identify the area.
- They are usually placed at least a week before the first radiation therapy treatment. The patient's skin may also be marked or tattooed with colored ink to help align and direct the radiation equipment.
- Patients with prostate problems who undergo IGRT using ultrasound should drink enough water about an hour before each treatment to keep their bladder full so that the prostate can be photographed or “seen” by the ultrasound machine.
- There is no specific preparation for IGRT, outside of routine radiation therapy preparation, which may be three-dimensional conformal radiation therapy, intensity-modulated radiation therapy, proton beam therapy, or stereotactic body radiation therapy (SBRT).
- See the IMRT page, the Proton Beam Therapy page, or the SBRT page for more information.
Special preparations needed for the procedure
They are generally performed on an outpatient basis. However, it's best to prepare to spend anywhere from half a day or more in the imaging department. You will be informed if you will need to have someone accompany you and drive you home after the procedure.
You may be told not to eat or drink anything after midnight before treatment. Ask your doctor if you should continue taking your regular medications on the day of treatment and if you should bring your medications with you to the procedure.
How is the procedure performed?
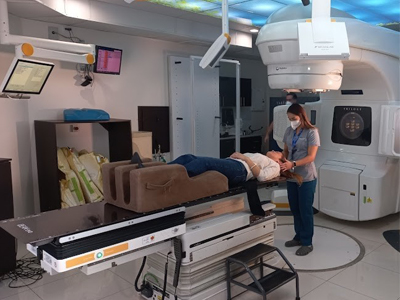
- At the beginning of each radiation therapy session, the patient is carefully positioned guided by the markings on the skin that define the treatment area. Devices may be used to help the patient maintain the correct position. Images are then taken using imaging equipment built into the radiation delivery machine or mounted in the treatment room. The doctor then reviews the images and compares them with those taken during the simulation. The patient may be repositioned and additional images may be taken. After any graduations have been made in the treatment plan and in the positioning of the patient, radiotherapy is then delivered. The imaging guidance process can be expected to add additional time to each radiation therapy session.

What does it feel like during and after the procedure?
Imaging performed before or during radiotherapy sessions is painless. During the radiation therapy session, you may see or hear the equipment moving around you during the imaging procedure. Patients sometimes notice a strange odor caused by the ozone produced by the linear accelerator. Some patients may also see a colored light when receiving their treatment; This event is especially true for patients receiving brain treatment. Side effects of radiation therapy include problems that occur as a result of the treatment itself as well as damage done by the treatment to healthy cells in the treatment area. The number and severity of side effects you experience depend on the type of radiation and dosage you receive and the part of the body undergoing treatment. You should talk to your doctor and nurse about any side effects you experience so they can help you manage them. Radiation therapy can cause early and delayed side effects. Early side effects occur during or immediately after treatment and usually disappear within a few weeks. Common early side effects of radiation therapy include tiredness or fatigue and skin problems. The skin in the treatment area may become more sensitive, red, irritated or swollen. Other skin changes include dryness, itching, peeling, and blistering.
Depending on the area undergoing treatment, other early side effects may include: hair loss in the treatment area mouth problems and difficulty swallowing problems eating and digestion diarrhea nausea and vomiting headaches tenderness and swelling in the area treatment urinary and bladder changes Delayed side effects, which are rare, occur months or years after treatment and are often permanent. They include: brain changes changes in the spine lung changes liver changes changes in the colon and rectum infertility joint changes lymphedema changes in the mouth secondary cancer There is a small risk of developing cancer from radiation therapy. After radiation therapy for cancer, you should undergo regular examination by your radiation oncologist to detect recurring and new cancers. Using techniques such as IGRT, imaging specialists are maximizing the cancer-destroying abilities of radiation therapy, while minimizing its effect on healthy tissues and organs and the side effects of the treatment itself.