Head and neck cancer
What is head and neck cancer?
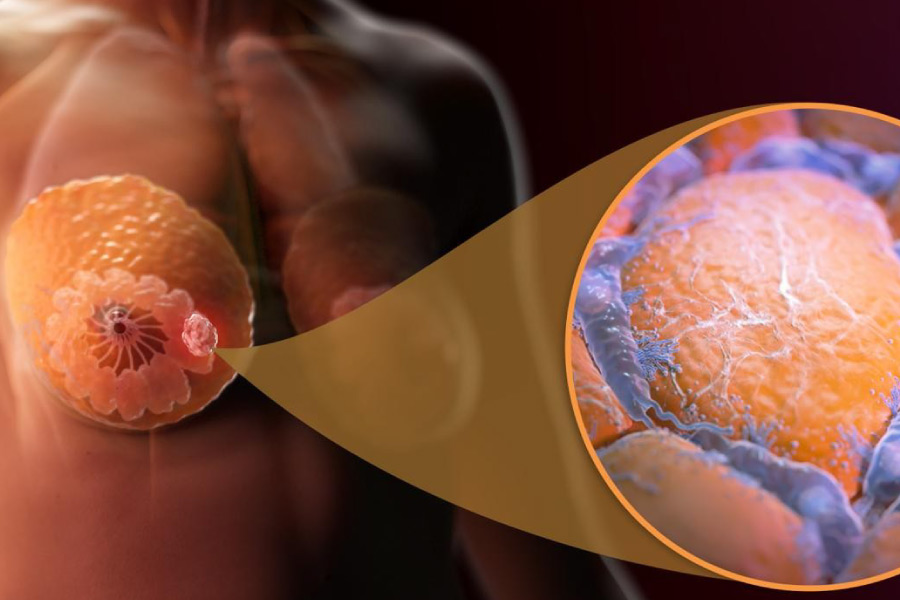
Head and neck cancers usually begin in the squamous cells that line the moist, mucous surfaces inside the head and neck (for example, inside the mouth, nose, and throat). Squamous cell cancer is often called squamous cell carcinoma of the head and neck. Head and neck cancers are, in turn, categorized according to the area of the head or neck in which they begin. These areas are: Oral cavity, Pharynx, Larynx, Paranasal sinuses, nasal cavity and, Salivary glands. Cancers of the brain, eye, esophagus, thyroid gland, as well as those of the scalp, skin, bones, and muscles of the head and neck are not generally classified as head and neck cancer.
Below are the details of some of these treatments:
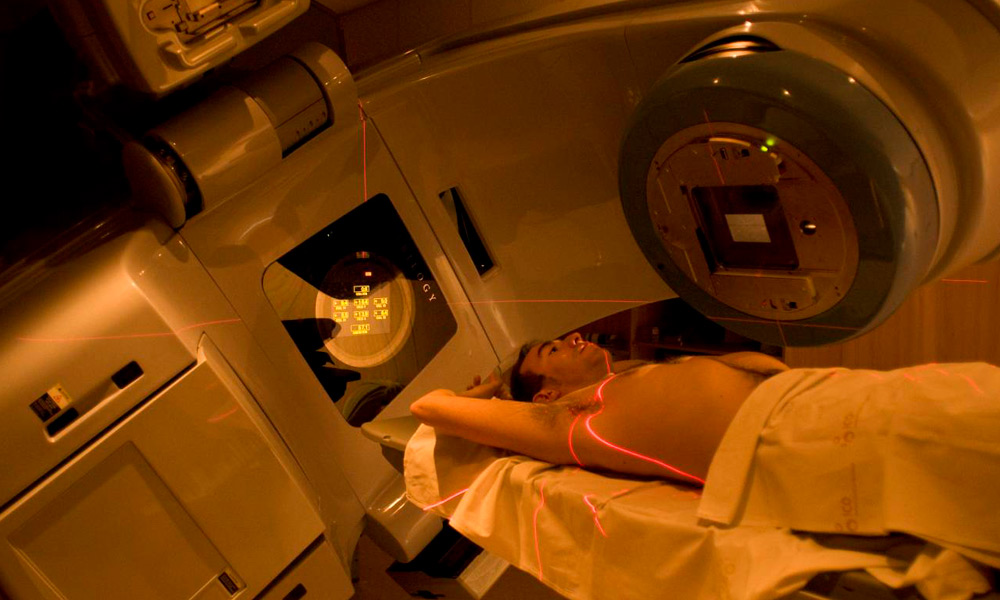
4D RADIOTHERAPY: Synchronizes treatment with the patient's breathing. This novel radiotherapy technique benefits patients with mobile tumor lesions by considering the patient's respiratory cycle from the moment of treatment planning.
To do this, the patient's image acquisition system not only takes the images at a given moment, but a series of images are obtained with the treatment area in the different positions it can adopt. In the planning system, these images can be represented by reproducing real movement, considering the patient's breathing.
This technique is used in injuries in which the treated area has a lot of involuntary mobility.
At the Siglo XXI Radiotherapy Medical Center we have extensive experience in the application of the latest technology for the treatment of injuries with radiotherapy. Through the use of IMRT or Intensity Modulated Radiotherapy, patients receive high doses of treatment in a millimetrically precise manner, this translates into a significant decrease in the amount of healthy tissue that is subjected to radiation doses, fewer side effects, better preservation of the healthy tissue and greater optimization of the patient's treatment time (fewer days of treatment than with conventional radiotherapy).
In addition to this, with the new 4D radiotherapy technology, the patient's respiratory cycles are considered in treatment planning. In this way, the equipment and doses will be calibrated to apply the treatment doses in the most optimal phases of the respiratory cycle, increasing the effectiveness and precision of the treatment of mobile tumors or lesions.
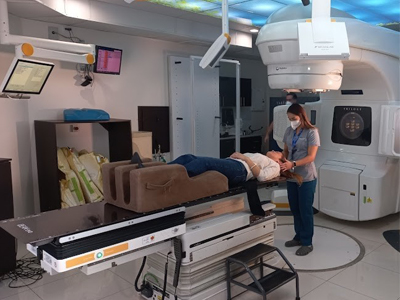
IMAGE GUIDED RADIOTHERAPY (IGRT): Image Guided Radiation Therapy or IGRT combines CT scan images with radiation therapy during each treatment session. This allows the area to be treated to be determined as precisely as possible and the areas surrounding the treatment area to be maximally protected.
What this technology does is place the patient at the exact point to irradiate the injury almost exclusively and not damage important organs; taking into account millimeter variables. This technology is not available in conventional radiotherapy systems.
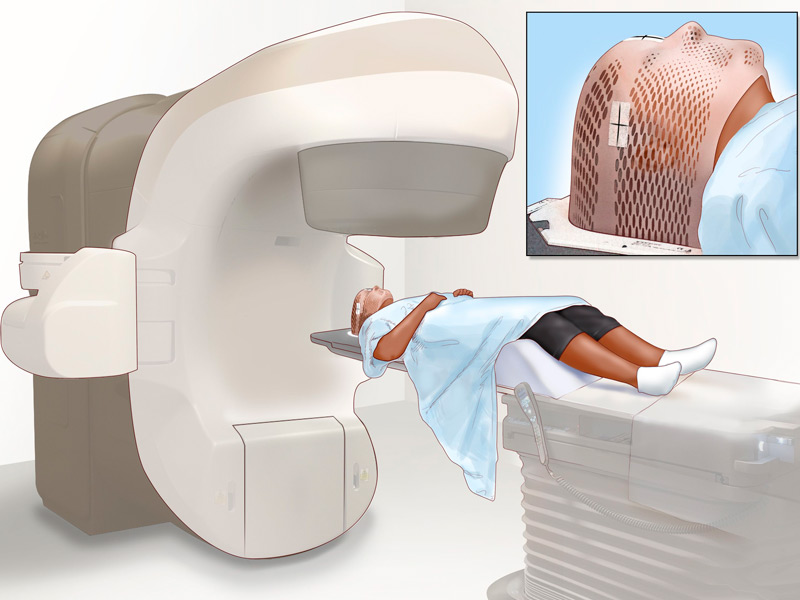
INTENSITY MODULATED RADIOTHERAPY (IMRT): Intensity Modulated Radiotherapy or IMRT is a technology through a computerized system that allows precise doses of radiation to be delivered to a tumor or specific areas within a tumor and reduce doses to healthy tissues.
This technology combined with the advantages of our linear accelerator offer the so-called Arc Therapy, which is the ability to irradiate an injury from 360 different angles, guaranteeing the highest quality treatment in an extremely short time (approximately 3 minutes). In this way, patient comfort and levels of precision are increased.
RADIOSURGERY: High doses in few treatments (1-5 sessions). Radiosurgery or SBRT is used in the treatment of small to medium-sized tumors.
Despite its name and compared to traditional radiation therapy, it is a non-surgical procedure that delivers highly focused radiation at much higher doses and in only one or a few treatments. This treatment is possible thanks to the development of highly advanced radiation technologies that allow the delivery of maximum doses within the target, while minimizing the dose received by the surrounding healthy tissue. The goal is to administer doses that destroy the tumor and achieve maximum local control.