Dr. Lorena Gallegos
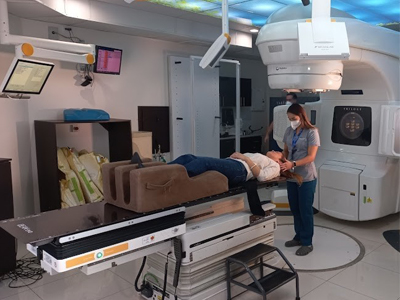
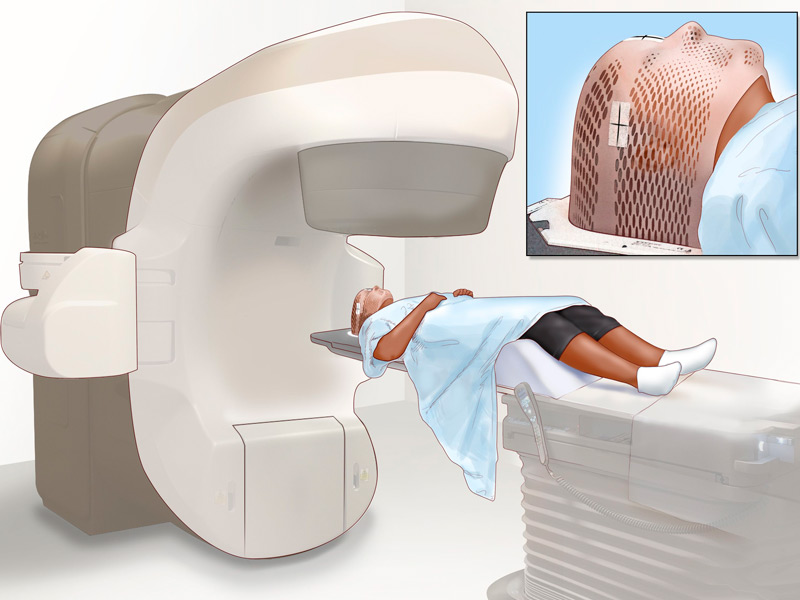
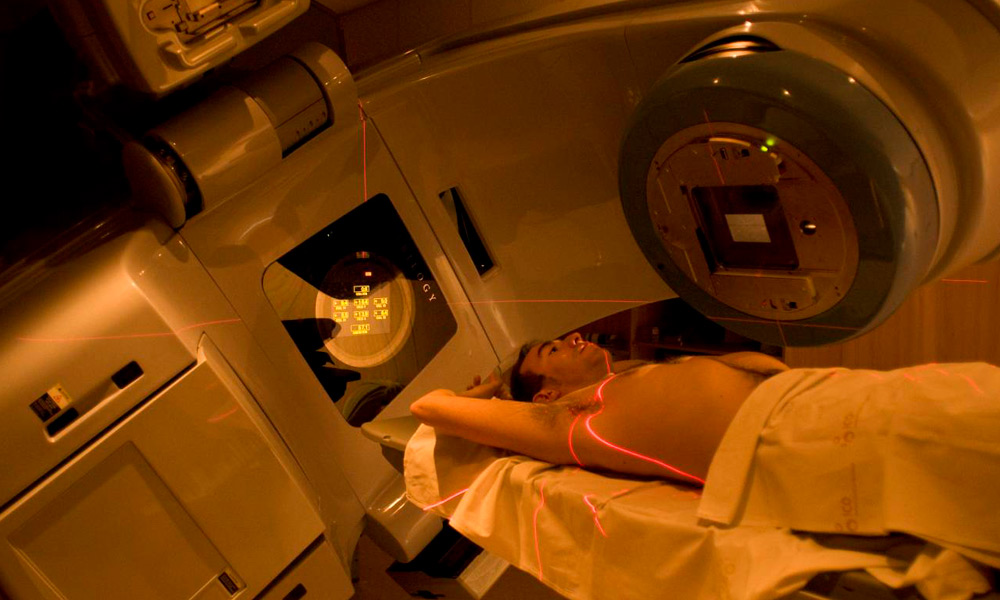
Oncologist and Radiation Therapist
Dr. Gallegos has extensive experience in radiation treatments, both radiotherapy and radiosurgery. He has experience in the management of multiple and localized injuries with novel approaches.

Academic education
BLS Course, Basic Support
San Jose, Costa Rica | Since 2019
Best of SABCS
San Jose, Costa Rica | Since 2018
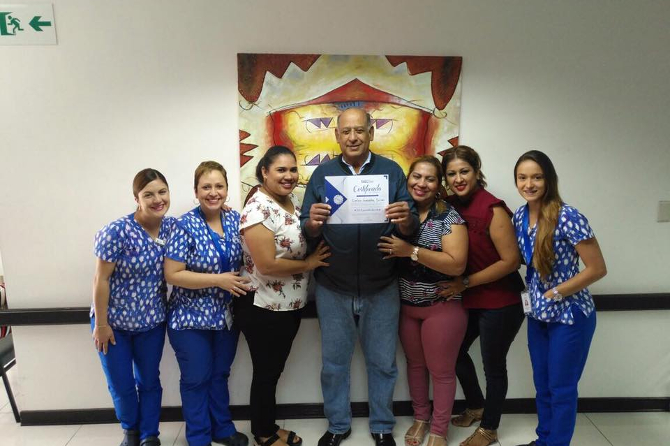
Cyberknife training and certification course
San Jose, Costa Rica | Since 2017
Regional training course on modern radiotherapy using linear accelerators
Argonne, Illinois, USA | Since 2016
Intraoperative radiotherapy course
San Jose, Costa Rica | Since 2012
Bachelor's and Doctorate in General Medicine and Surgery
University of Costa Rica | Since 2003
Specialty in Oncological Radiotherapy
University of Costa Rica | Since 2003
Rotation at National Cancer Institute
Mexico City, DF | Since 2003
Work experience
Postgraduate professor of oncological radiotherapy
University of Costa Rica | 2009 - Current
Assistant physician specialist in radiotherapy oncology
San Juan de Dios Hospital. Hospital and Mexico | 2003 - Current
Resident doctor of internal medicine and oncological radiotherapy
Mexico Hospital | 1999 - 2003
General Assistant Physician
United Supermarkets
1998 - 1999
Doctor and coordinator of the EBAIS of Bejuco de Nandayure
Guanacaste, Ministry of Health | 1997 - 1998